The NR 503 final exam answers are the key to unlocking success in the NR 503 course. This comprehensive guide provides everything you need to know to prepare for and ace the exam, including an overview of the exam format, key concepts and theories, nursing process and patient care, evidence-based practice, communication and collaboration, ethical and legal issues, health promotion and disease prevention, nursing leadership and management, and case studies and practice scenarios.
With this guide in hand, you’ll be well-equipped to tackle the NR 503 final exam with confidence and achieve your academic goals.
Overview of NR 503 Final Exam: Nr 503 Final Exam Answers
The NR 503 final exam serves as a comprehensive assessment of students’ knowledge and skills acquired throughout the course. It evaluates their understanding of advanced nursing practice concepts, research methods, and their application in clinical practice.
The exam consists of multiple-choice questions, short answer questions, and essay questions. It is typically 3 hours long and carries a significant weight in the overall course grade. The grading criteria vary depending on the specific exam format and the instructor’s guidelines.
Key Concepts and Theories
The NR 503 course introduces various key concepts and theories that form the foundation of nursing practice. These concepts and theories provide a framework for understanding the complex healthcare environment and guide nurses in delivering evidence-based, patient-centered care.
The application of these concepts and theories is essential for nurses to effectively assess, diagnose, plan, implement, and evaluate patient care. They enable nurses to understand the physiological, psychological, social, and cultural factors that influence patient health and recovery.
Nursing Process
The nursing process is a systematic and evidence-based approach to patient care that incorporates the following steps:
- Assessment: Gathering data about the patient’s health status and needs.
- Diagnosis: Identifying the patient’s health problems or potential risks.
- Planning: Developing a plan of care that Artikels interventions to address the patient’s needs.
- Implementation: Carrying out the plan of care and monitoring the patient’s response.
- Evaluation: Assessing the effectiveness of the plan of care and making necessary adjustments.
Health Promotion and Disease Prevention
Health promotion and disease prevention are key concepts in nursing that focus on maintaining and improving health and preventing illness. Nurses play a crucial role in promoting healthy lifestyles, educating patients about disease risks, and implementing preventive measures.
Evidence-Based Practice
Evidence-based practice is an approach to healthcare that uses the best available evidence to guide clinical decision-making. Nurses use research findings, clinical guidelines, and other evidence-based resources to inform their practice and improve patient outcomes.
Cultural Competence
Cultural competence is the ability to understand and respond to the cultural needs of patients. Nurses must be aware of the cultural beliefs, values, and practices that influence health behaviors and healthcare outcomes.
Interdisciplinary Collaboration
Interdisciplinary collaboration is essential in providing comprehensive and coordinated patient care. Nurses work with other healthcare professionals, such as physicians, social workers, and pharmacists, to ensure that patients receive the best possible care.
Ethics and Legal Issues
Ethical and legal issues are inherent in nursing practice. Nurses must be aware of the ethical principles and legal regulations that govern their practice and make ethical decisions in the best interests of their patients.
While studying for the NR 503 final exam answers, I stumbled upon an interesting article on medic response 7 per rule . It’s a fascinating concept that relates to the NR 503 course material in unexpected ways. By understanding the medic response rule, we can gain insights into the efficiency and effectiveness of emergency medical services, which is crucial for nurses in providing optimal patient care.
This knowledge will undoubtedly enhance my preparation for the NR 503 final exam answers.
Nursing Process and Patient Care
The nursing process is a systematic, problem-solving approach to patient care. It consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The nursing process is used to identify patient problems, develop and implement a plan of care, and evaluate the effectiveness of the care provided.
The nursing process can be applied to any patient care situation. For example, a nurse might use the nursing process to care for a patient with a new diagnosis of diabetes. The nurse would first assess the patient’s condition, including their blood sugar levels, diet, and exercise habits.
The nurse would then diagnose the patient with diabetes and develop a plan of care that includes teaching the patient about diabetes, monitoring their blood sugar levels, and providing them with medication.
Assessment
The assessment phase of the nursing process involves collecting data about the patient’s health status. This data can be collected from a variety of sources, including the patient’s medical history, physical examination, and laboratory tests. The nurse will use this data to identify the patient’s problems and develop a plan of care.
Diagnosis
The diagnosis phase of the nursing process involves identifying the patient’s problems. The nurse will use the data collected during the assessment phase to identify the patient’s problems. The nurse will then develop a list of nursing diagnoses that describe the patient’s problems.
Planning
The planning phase of the nursing process involves developing a plan of care for the patient. The plan of care will include a list of goals and interventions that are designed to address the patient’s problems. The nurse will work with the patient to develop the plan of care.
Implementation
The implementation phase of the nursing process involves carrying out the plan of care. The nurse will implement the interventions that are listed in the plan of care. The nurse will also monitor the patient’s progress and make any necessary adjustments to the plan of care.
Evaluation
The evaluation phase of the nursing process involves evaluating the effectiveness of the plan of care. The nurse will evaluate the patient’s progress and make any necessary changes to the plan of care. The nurse will also document the patient’s progress in the patient’s medical record.
Evidence-Based Practice
Evidence-based practice (EBP) is a systematic approach to nursing care that utilizes the best available research evidence, clinical expertise, and patient values to make informed decisions about patient care.
EBP involves:
- Finding research evidence
- Evaluating the evidence for validity, reliability, and applicability
- Applying the evidence to nursing practice
Finding Research Evidence
Nurses can find research evidence from a variety of sources, including:
- Databases (e.g., PubMed, CINAHL)
- Journals
- Conference proceedings
- Books
Evaluating Research Evidence
When evaluating research evidence, nurses should consider the following:
- The study design
- The sample size
- The results
- The conclusions
Applying Research Evidence to Nursing Practice
Once nurses have evaluated research evidence, they can apply it to nursing practice in a variety of ways, including:
- Developing new policies and procedures
- Changing existing policies and procedures
- Educating patients and families
- Making decisions about patient care
Communication and Collaboration
Effective communication and collaboration are vital in nursing. They ensure accurate information exchange, enhance patient care, and foster a positive work environment.
Nurses communicate with patients, families, and other healthcare professionals to gather information, provide updates, and coordinate care. Clear and empathetic communication builds trust, reduces errors, and improves patient satisfaction.
Strategies for Effective Communication
- Use active listening skills: Pay attention, ask clarifying questions, and reflect on what you hear.
- Speak clearly and concisely, using language appropriate for the audience.
- Be mindful of non-verbal cues, such as body language and tone of voice.
- Respect cultural and linguistic differences.
- Document communication accurately and promptly.
Collaboration with Healthcare Team
Collaboration is essential for providing comprehensive patient care. Nurses work with physicians, social workers, pharmacists, and other professionals to develop and implement care plans.
- Participate in interdisciplinary team meetings.
- Share patient information and updates.
- Seek input from other professionals.
- Coordinate care transitions and referrals.
- Maintain a positive and respectful work environment.
Ethical and Legal Issues
In the dynamic field of nursing, ethical and legal considerations play a pivotal role in guiding practice and ensuring patient well-being. Understanding these principles and regulations empowers nurses to make informed decisions that uphold both ethical obligations and legal requirements.
Ethical principles, such as autonomy, beneficence, non-maleficence, and justice, serve as the foundation for nursing practice. Autonomy emphasizes respecting patients’ rights to make decisions about their own care. Beneficence entails acting in the best interests of the patient, while non-maleficence dictates avoiding harm.
Justice ensures fair and equitable access to healthcare resources.
Legal Regulations
Nurses must adhere to legal regulations governing their practice, including federal and state laws, agency policies, and professional standards. These regulations provide a framework for safe and ethical patient care. For example, the Nurse Practice Act defines the scope of practice for nurses in each state, outlining the activities they are authorized to perform.
Applying Ethics and Law to Patient Care
Applying ethical principles and legal regulations to patient care requires nurses to engage in critical thinking and ethical reasoning. They must consider the patient’s values, preferences, and best interests while navigating complex legal and ethical issues. Nurses often consult with ethics committees or legal counsel for guidance in challenging situations.
Ethical Dilemmas
Nurses may encounter ethical dilemmas where there is no clear right or wrong answer. For instance, they may face conflicts between patient autonomy and the duty to protect the patient from harm. Resolving these dilemmas requires careful consideration of ethical principles, legal implications, and the specific circumstances of the case.
Health Promotion and Disease Prevention
Nurses play a crucial role in promoting health and preventing disease within communities. They serve as educators, advocates, and healthcare providers, working to empower individuals and families to make informed decisions about their health. By understanding the principles of health promotion and disease prevention, nurses can effectively guide individuals towards healthier lifestyles and reduce the risk of developing chronic diseases.
Strategies for Promoting Healthy Lifestyles
Nurses can promote healthy lifestyles through various strategies, including:
- Providing education on healthy eating habits, physical activity, and stress management.
- Encouraging regular check-ups and screenings to detect and prevent health problems early on.
- Advocating for policies and programs that support healthy choices, such as access to healthy food and safe places for physical activity.
- Collaborating with community organizations to offer health promotion programs and resources.
Strategies for Preventing Disease
Nurses can also contribute to disease prevention by:
- Identifying individuals at risk for developing certain diseases based on their family history, lifestyle, and other factors.
- Providing tailored interventions to reduce risk factors, such as smoking cessation programs or cholesterol management plans.
- Educating patients about the importance of immunization and vaccination.
- Promoting early detection and treatment of chronic diseases to prevent complications and improve outcomes.
Nursing Leadership and Management
Nurses play a pivotal role in healthcare leadership and management, utilizing their clinical expertise and understanding of patient needs to shape healthcare delivery and improve patient outcomes. They are instrumental in driving quality improvement initiatives, fostering interdisciplinary collaboration, and advocating for patients’ rights and well-being.
Effective nursing leaders and managers apply principles of leadership and management to guide their practice, empowering their teams, promoting a positive work environment, and ensuring the delivery of high-quality patient care. These principles include:
Vision and Mission Alignment
Nursing leaders align their leadership approach with the organization’s vision, mission, and values, ensuring that nursing practices contribute to the overall goals and objectives of the healthcare system.
Communication and Collaboration
Effective communication and collaboration are essential for successful nursing leadership. Nurses foster open communication channels, actively listen to their team members and patients, and facilitate collaboration among healthcare professionals to enhance patient care.
Decision-Making, Nr 503 final exam answers
Nurses make informed decisions based on evidence-based practice, ethical principles, and patient-centered care. They consider multiple perspectives, weigh risks and benefits, and involve stakeholders in the decision-making process.
Resource Management
Nursing leaders manage human, financial, and material resources effectively to optimize patient care and achieve organizational goals. They allocate resources strategically, ensure efficient use of equipment and supplies, and advocate for adequate staffing levels.
Quality Improvement
Nurses continuously strive to improve the quality of patient care through ongoing evaluation, monitoring, and implementation of evidence-based practices. They identify areas for improvement, develop and implement quality improvement initiatives, and measure outcomes to assess effectiveness.
Mentorship and Development
Nursing leaders mentor and develop their team members, providing guidance, support, and opportunities for professional growth. They recognize the importance of investing in their staff and fostering a culture of continuous learning.
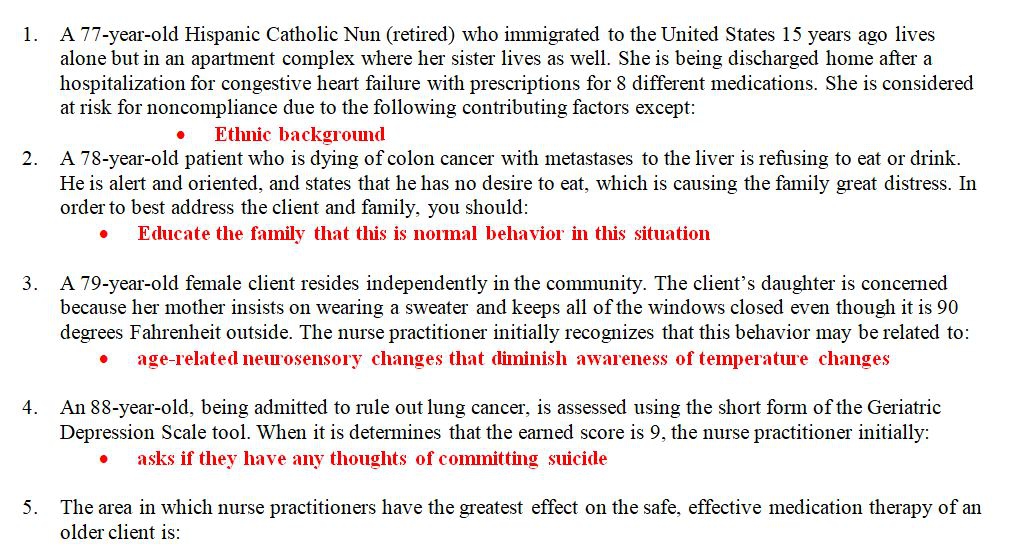
Case Studies and Practice Scenarios
Case studies and practice scenarios provide opportunities to apply the concepts learned in NR 503 to real-world nursing situations. By analyzing and responding to these scenarios, students can develop their critical thinking and decision-making skills.
To analyze a case study or practice scenario, students should first identify the key issues and concepts involved. They should then consider the different perspectives of the individuals involved and the potential consequences of different actions. Based on this analysis, students can develop a plan of care that is evidence-based and patient-centered.
Analyzing Case Studies and Practice Scenarios
- Identify the key issues and concepts involved.
- Consider the different perspectives of the individuals involved.
- Consider the potential consequences of different actions.
- Develop a plan of care that is evidence-based and patient-centered.
Key Questions Answered
What is the format of the NR 503 final exam?
The NR 503 final exam is a comprehensive exam that covers all of the major concepts and theories covered in the course. The exam is typically three hours long and consists of multiple-choice, short answer, and essay questions.
What are some tips for preparing for the NR 503 final exam?
The best way to prepare for the NR 503 final exam is to start studying early. Begin by reviewing your class notes and textbooks. You should also practice answering multiple-choice, short answer, and essay questions. Additionally, it is helpful to form a study group with other students in the class.
What are some common topics covered on the NR 503 final exam?
Some common topics covered on the NR 503 final exam include the nursing process, evidence-based practice, communication and collaboration, ethical and legal issues, health promotion and disease prevention, and nursing leadership and management.